Greg Thorkelson, MD with Ryan Reagan, PhD(c), LPC

This week’s blog on mental health will focus on bipolar disorder. Bipolar Disorder effects about 4% of the population according to the most recent estimates by the National Institutes of Mental Health. We will be giving a good amount of space and attention to the subject this week to help bring clarity to a disorder that can be frustratingly illusive in diagnosing. If you are unfamiliar with bipolar disorder, a casual reading can start to feel like a mystifying set of paradoxes—how can an individual experience depression and mania at the same time? How is that this disorder has telltale features that make the diagnosis quite easy, and at the same time we read that it is often misdiagnosed? One researcher claims that it is over-diagnosed, another claims that it is terribly under-diagnosed.
Unfortunately, because of this confusion, it often goes untreated or may receive the wrong treatment. This is highly problematic for many reasons. One, the condition is believed to be lifelong, and it can be debilitating. 83% of individuals diagnosed with bipolar are considered to have severe symptoms, and part of this is probably due to the length of time that it can take to pin down a diagnosis and get the proper treatment. As with any chronic medical condition, left untreated it will likely get much worse before it gets better. The good news is that it can “get better,” once treated it can be a manageable condition much like diabetes.
Another reason contributing to underdiagnosis is that people tend to seek help during the depressive phase only. Milder symptoms in the manic phase, referred to as hypomania may go unnoticed or mistaken to a rebound to normal mood following depression. Severe manic symptoms on the other hand are very noticeable and often lead to hospitalization. Unfortunately, this sometimes comes about through interface with community law enforcement. This is even more reason that it is important to identify the disorder as early as possible and begin the proper treatment. The risks tend to accumulate when the condition goes untreated.
Bipolar disorder involves a dysregulation of the mood cycle. To help illustrate this, consider the picture below from The Lancet:
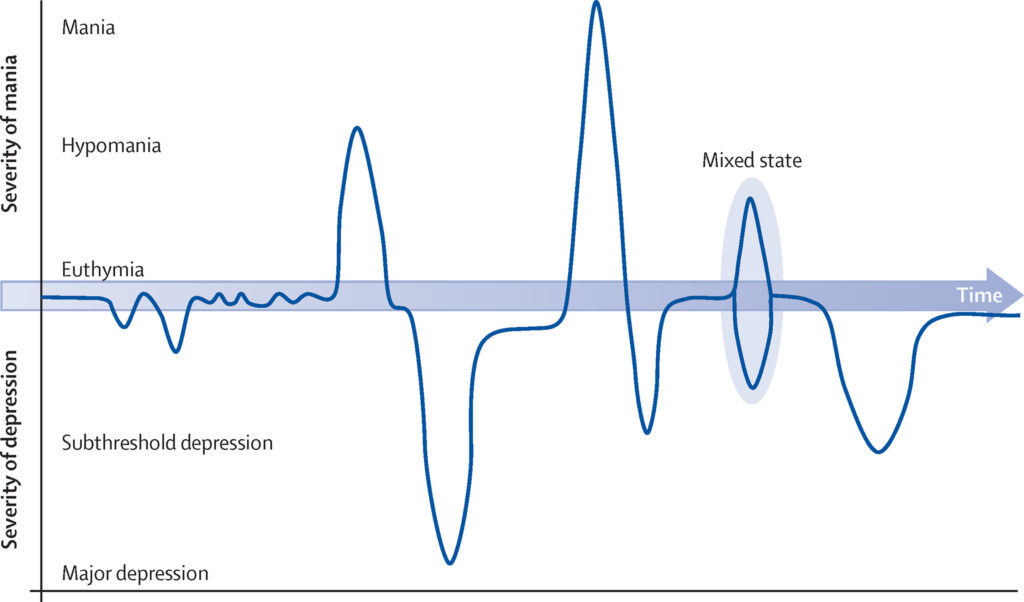
This picture provides a visual depiction of the mood cycle associated with bipolar disorder. The two peaks represent the manic phase and the depressive phase. Mania involves an elevated mood; depression is depicted by the lower half of the figure. You will also notice that “mixed state” is listed on the graph. One of the things that makes diagnosis challenging is that a person suffering from bipolar disorder may present with symptoms of depression and mania simultaneously—this might look like a deeply agitated or irritable depression. Mood lability is also common in this state. The person may go from elevated—giddy, grandiose, to sobbing a few moments later.
You will notice that below the peaks and are areas referred to as “subthreshold.” One of the reasons that bipolar disorder is difficult to diagnose is that the mood cycle often hits places short of full-blown depression or mania. Furthermore, Eugene Rubin MD, notes that many of the symptoms that distinguish bipolar disorder also occur commonly in the general public—occasional bouts of irritability, insomnia, increased interest in sexual activity, and pressured speech. Even symptoms of psychosis have been observed in individuals with no previous psychiatric diagnosis.

What is the difference in bipolar I and bipolar II?
You may have done some research or heard something in the news that “so and so (often a celebrity) was diagnosed with bipolar II disorder.” To put it simply, the difference in the two disorders is the intensity of symptoms. This should not be taken to suggest that bipolar II is any less severe, it can be equally debilitating. The dysregulation of the mood cycle can make it difficult to maintain a job, increase conflict with family and friends, and lead to impulsive risk taking. It might be helpful to think of it this way—bipolar II may be less likely to draw attention.
You may have noticed that a lot of these cases that draw public attention, involve celebrities and artists. There is a reason for this, during bouts of euphoria that stop short of mania, creativity and productivity may show a marked increase. Many historical writers and artists were believed to suffer from bipolar—Hemmingway is often mentioned. It was said that Handel wrote the Messiah in under 3 weeks, a feat that baffles modern composers. More recently, Kanye West was in the news, and regardless of your opinion, it was a sad spectacle to watch talent so clearly diminished to spectacle.
It is one thing to call yourself the greatest living artist, it is altogether different to announce your presidential run, intermittently sobbing, and making very little sense. Not long after this his partner separated. And this is one of the tragic consequences of having a family member with bipolar disorder. They can be alternately charming, productive, exhilarating, moody, brooding, and irritable, which again happens in all of us. The problem with bipolar disorder is that it becomes exhausting to be around because the symptoms can be more exaggerated and constantly shifting. It can be difficult to keep family members safe from exceptionally poor judgment, especially in a culture that prides risk taking.
The distinguishing feature of bipolar I is mania. In fact, bipolar disorder can be diagnosed based on a single episode of mania without any history of depression. The average age of onset for bipolar disorder is 25. Adolescents and individuals in their early twenties may be experimenting with drugs, away from close friends and family who would recognize out of character behavior, and for woman this may be the window of time for first pregnancy. It is well documented, that first pregnancies can trigger first episodes of mania. The first indication of a bipolar disorder may appear abruptly without much notice.
Bipolar II, on the other hand, does not have mania. Again, mania is an episode of elevated mood that is often of an intensity that it often draws concern or attention. A person with a bipolar II diagnosis does not experience elevated mood episodes that reach this intensity. The episode is referred to as hypomania, meaning “below” mania. What is often confusing for both patients and those treating the disorder, is that people with bipolar I can also experience hypomanic episodes, falling short of a manic episode. Those with bipolar II however, have never crossed into mania. Individuals with bipolar II experience depressive episodes along with hypomania. While a person with bipolar I can have a single episode of mania, the vast majority also experience frequent episodes of depression.
Symptoms associated with bipolar disorder.
So far, we have spent time explaining that bipolar disorders are defined by episodes of mood dysregulation. The symptoms of these episodes are described below:
Manic Symptoms: elevated or euphoric mood, pressured speech (excessive talkativeness), increased self-esteem or grandiosity, decreased need for sleep, increased energy level, agitation, racing thoughts, poor attention, hypersexuality, increased risk-taking behavior, intense creativity, and possible psychosis.
Depressive Symptoms: feeling intense sadness, hopelessness, low mood, loss of interest in normally enjoyed activities, insomnia or hypersomnia (over-sleeping), loss of appetite or over eating, psychomotor retardation (moving more slowly) or psychomotor agitation (feeling fidgety and restless), feelings of worthlessness or inappropriate guilt, recurrent thoughts of death or suicidal ideation, plans, or attempts.
Again, these symptoms can occur in anyone from time to time. But, in order to consider it an “episode” a certain number of symptoms need to be present together and for a certain period of time. For example, an episode of Major Depression requires 5 of the 9 symptoms to be present, most of the day and for at least 2 weeks; and one of the first two symptoms must be present—depressed mood or loss of interest. While this may sound arbitrary, it helps professionals identify whether it is a mood episode. The symptoms of depression can go with other medical disorders—thyroid disease, for example. Therefore, if the symptoms of depression were present, but without the mood symptom, the provider would be inclined to consider whether there was a medical condition that could account for the symptoms.
In distinguishing between mania and hypomania, mental health providers look to the intensity and duration of symptoms. Manic episodes are more intense, grandiosity can tip into psychosis. This might look like—“I’m going to write the year’s best novel” (possible) versus “I’m getting secret messages from God and I need to transmit this to save souls” (possible, but cause for concern). Joking aside, there is a serious point there. Many people with bipolar disorder report intense feelings of spirituality at times, which sometimes referred to as “hyper-religiosity” or “religious preoccupation.”
Along with intensity of symptoms, the other distinguishing feature is duration. Hypomania typically lasts a few days (3-4) whereas mania lasts at least a week or longer. Again, the symptoms must be occurring at the same time. Feeling irritable, having decreased sleep for sleep, and increased talkativeness for a period of days around a major work project would not qualify for hypomania. If euphoric mood, grandiosity, or unusual risk taking accompanied the other symptoms it might qualify. This is because stressful life events can easily trigger episodes.
The Overlap with Substance Use.
It is unfortunate that the onset of bipolar also occurs at the same time when many are also experimenting with casual and social use of drugs and alcohol. Alcohol is a depressant and will tend to have a depressant effect on mood. The overlap between a substance abuse disorder and mental health disorder is no referred to as co-occurring disorder (formerly dual diagnosis). Stimulants like cocaine and methamphetamine have the opposite effect. ER doctors will report that there is very little difference in the presentation of person experiencing stimulant intoxication versus mania. If that person is young and has no psychiatric history and happened to be using substances it can be difficult to determine cause.
As a result, a bipolar diagnosis might be missed. There is a reluctance to apply a diagnosis that carries this magnitude on a single observation. There might also be reluctance on the part of the patient to be forthcoming with details due to the stigma associated with mental illness, and the minimizing that sometimes goes with substance abuse. The patchwork nature of our medical system and the tendency of people to move around the country in their late teens and early 20’s makes it likely that someone has seen multiple doctors. Arriving at a correct diagnosis of bipolar disorder may take time or extensive review of records for a doctor to spot the pattern.
The importance of identifying the disorder early and starting treatment cannot be overstated. There are risks involved in misdiagnosis. Certain medications used to treat depression can also increase manic symptoms. This is sometimes the clue that there is a bipolar disorder present. It is not uncommon to treat bipolar with antidepressants, but the individual also is usually prescribed a mood stabilizer like lithium or Depakote. A mood stabilizer helps to bring the mood cycling to a more manageable range. The other reason to start treatment early is that the disorder tends to worsen if untreated. The stress of lost employment, family conflict, and worsening health can increase the toll of suffering.

What can you or friends and family do?
The writer April Michael provides some helpful advice from her own experience with bipolar disorder. First, see a psychiatrist and ask for enough time to really talk. The psychiatrist needs detail. Ask questions, discuss past experiences, and share openly and honestly. The Nexus Group strives to provide patients with the time necessary for a thorough assessment and ongoing treatment. Bipolar is a chronic condition and you are best served by establishing a healthy relationship where a doctor can observe your symptoms over time.
Second, have a physical workup. Again, underlying health conditions can worsen or contribute to symptoms. Additionally, research indicates that individuals with bipolar have higher risk for comorbid medical conditions like Type II diabetes. As with any chronic condition, what is good for the body is also good for mental health. Diet and exercise can have a significant impact on stress, and lower stress decreases the likelihood of symptoms.
If possible, provide your doctor with medical records and family history. It is believed that genetics plays a role in the development of bipolar disorder. Certainly, knowing that close family members carried the diagnosis will help improve the accuracy of diagnosis. Also, it is tremendously helpful to include family and friends as supports. Friends and family can help to ensure that medications are taken as prescribed. One of the all-too-common features we observe as mental health providers is that the patient discontinues medications believing that they were no longer necessary. This tends to lead to relapse in symptoms.
Finally, consider joining a support group or an advocacy group. Bipolar is a common condition and having social supports that understand the challenges that come with managing the disorder helps. If you can assemble a support system, establish a good relationship with a mental health provider, maintain a medication regimen, and include diet and exercise, this condition can be managed. You have a right to hope.

